Healing to the bone
Updated: 2018-11-23 07:12
(HK Edition)
|
|||||||
A team of scientists from HK and the mainland made a breakthrough, pulling off a successful cross-boundary collaboration with an unorthodox way to heal the bone. Dara Wang reports.
The Marvel Comics superhero Mr Immortal can heal just about anything - at the high price of suffering a near mortal injury himself. Hu Jinlian, a professor at the Institute of Textiles and Clothing at the Hong Kong Polytechnic University, can do something like that for patients with bone injuries - without risking near fatal consequences.
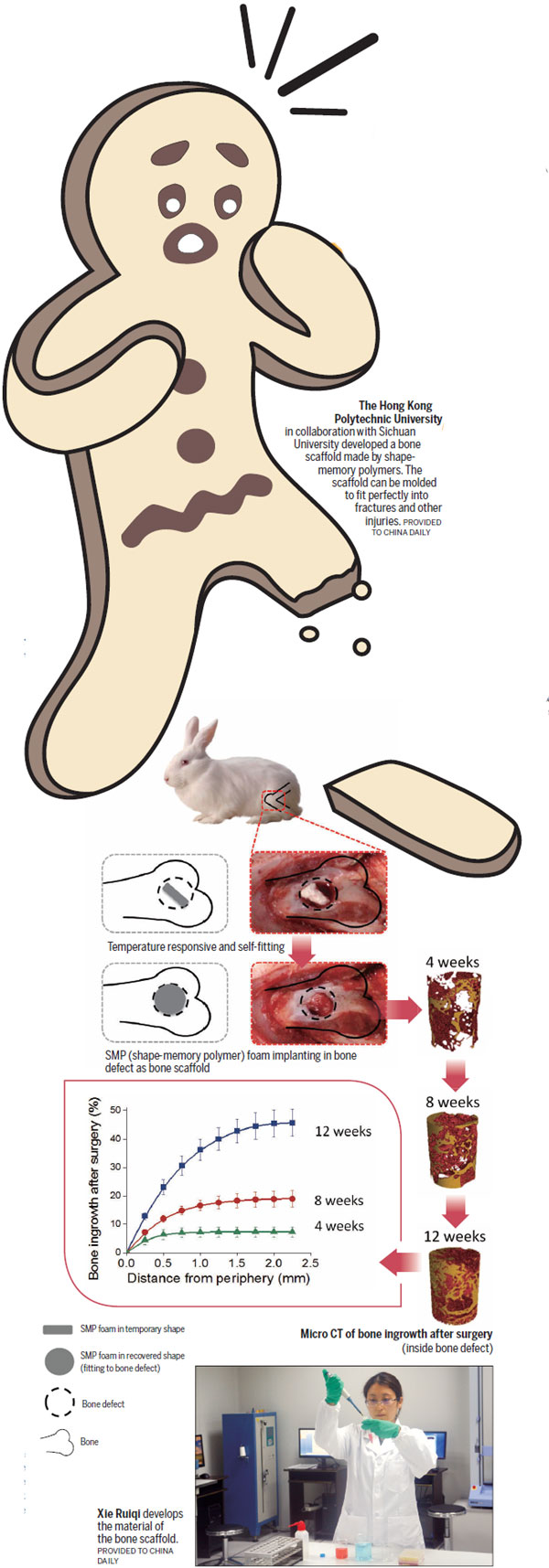
She and her team developed a bone scaffold for healing injuries. It can be operated through minimally invasive surgery and fit the bone injury perfectly, supporting the bone and helping to heal the injuries. It works even for bone injuries larger than 5 millimeters in diameter that cannot not self-heal.
There are two major components to the device - polyurethane (PU), which is used for making resilient foam, and hydroxyapatite (HA), which already occurs naturally in bones.
PU is a kind of polymer, commonly used for seats and for the durable wheels on roller coasters and shopping carts. It has shape-memory function. Researchers compressed the PU foam into a small shape, tiny enough to be operated through minimally invasive surgery. Then they inserted it around the bone damage. Within a minute, after being soaked in a saline solution at 40 C, the foam returned to its original shape, molding itself to the damaged area precisely, Hu says.
The solution works for fractures, breaks and other defects of bone structure.
HA gives teeth and bones their hardness. It improves the hardness of the scaffold in the same manner, making it hard enough to support the bone.
Another function of HA is to help new cells grow and restore injured bones much more quickly, says Hu. As HA is a component of bone, bone cells recognize HA as "brothers" and cling onto them.
The porous structure of the scaffold provides "tubes" for the new cells to worm their way inside, find their "brothers", and proliferate, Hu says.
Sixty-percent of the scaffold is composed of pores, and 99 percent of the pores on the device are interconnected. The pores are only 670 m in diameter, close to what we find in natural bones.
Lab experiments were carried out on 18 rabbits with knee defects. Nine rabbits were implanted with the scaffold. The rest, the control group, were given no implants.
Twelve weeks later, researchers found rabbits that had received the implants showed a 46-percent increase in bone mass. That was nearly double the regrowth among the rabbits that did not receive the implants. There were also significantly more new blood vessels in the test group than were found in the control group.
Alternatives
The Journal of Tissue Engineering cites more than 15 million cases of bone fractures or defects caused by misadventure or disease every year around the world. Defects caused by removal of bone tumors or fractures larger than 5 millimeters in diameter rarely heal without surgical intervention, says Guo Xia, associate professor of the Department of Rehabilitation Sciences at PolyU. She is the joint principal researcher of the study and worked as an orthopedist for eight years before joining the university.
Guo remarked that current standard practice for repairing bone injuries is the autograft. Autograft involves removing healthy bone from one part of the body and using it to repair the damaged bone. "It works quite well, while it's a painful procedure, and let's face it there are no 'spare parts' or non-essential bones in the human body," Guo says. Removing healthy bones causes pain. There are risks of infection and other complications. Problems can flare up where healthy bone is removed.
Another procedure for repairing damaged bones uses shape-memory alloys. These are able to retain their original form under stimulus. They're not perfect. Shape-memory alloys don't fit perfectly into damaged areas, Guo says. The surgeon has to smooth rough edges around the repair. Alternatively the alloy may be reduced to tiny fragments. Even then, there is no perfect fit. Pain and other discomfort is inevitable and there's also a risk of infection.
By contrast, the shape-memory bone scaffold creates a perfect fit, Guo says. It can be implanted using minimally invasive surgery. The risk of pain and secondary infection is minimized and hospital stays are shortened, she says.
The objective is that the scaffold supports the injured area, and stimulates regrowth of bone. Hu noted that the ideal scaffold should degrade in the body over time, after the bone heals.
The natural degradation of the device noted in the animal experiments proceeded slowly during the 12 weeks. It will take years to figure out how long it takes for complete degradation and only then will the researchers be able to determine whether it has any side effects on the human body.
Guo says she was satisfied with the slowness. If degradation proceeds too fast, there is a risk of acids being released, changing the pH. That would pose a risk of tumors later on, Guo says.
Shooting for the moon
The development of the bone scaffold is another case where cross-boundary collaboration played an important role.
When they started the project in 2013, Guo with her medical background didn't take the project seriously at first. She thought it was shooting for the moon. Then along came Xie Ruiqi - Hu's doctoral student from Renqiu, Hebei province who, 27 years old at that time, took up the project for her doctoral research.
Xie, who studied chemical engineering for her bachelor's and master's degrees on the Chinese mainland, came to Hong Kong in 2012, wishing to explore uncharted waters, both in life and in the academic field.
The team decided to use PU as the base material at an early stage as the material's shape-memory function fit their expectation on an ideal scaffold. But PU is not hard enough to support the bone.
The challenge was to find a way to make PU stronger and more durable, without affecting its biocompatibility and other features.
Xie worked from 9 am until midnight, seven days a week. She kept her paperwork in the hallway to save the 10-minute walk from her office.
"My academic background is not as strong as my schoolmates. I am not smart, either. All I can do is work diligently," Xie says.
The team used 10 months to decide on PU and HA and used another 10 months to find a way to combine the two. After extensive experiments, they found the solution - activating the bonds responsible for chemical interactions within the PU and replacing those connection points or netpoints with HA.
The PU/HA combination provided the stable performance the researchers were seeking. The combination remained stable even after solvents were added to create a foamy substance.
On the day they made the breakthrough on the combination, Xie was not filled with joy, nor did the calm scientist from a humble background treat herself to a big meal. "It was just a normal day to me. I did not celebrate. I knew the project still had a long way to go," Xie recalled with a calming smile.
They finished the material development at PolyU, where the university offered equipment and labs free of charge. Next, they needed to carry out animal tests. There came another problem.
They needed advanced equipment and expert guidance in animal selection, which exceeded what PolyU could provide for free. They did get a research fund at HK$3 million. However, it was granted by the Shenzhen Government Basic Research Fund, which was not allowed to be spent across the boundary in Hong Kong.
The terms of the grant stipulated that the laboratory must be on the mainland. In May this year, that rule was changed. Still, only grants for national key technology programs can be used in Hong Kong.
Back in 2008 when an earthquake struck Wenchuan area of Sichuan province, a lot of Hong Kong institutions was deeply involved in post-disaster rescues and recovery work. PolyU is one of them. They helped victims suffering from multiple bone fractures. So naturally, when Hu needed a partner on the mainland, an invitation was sent to Professor Qin Tingwu and his team at West China Hospital, Sichuan University.
The animal tests were done using the advanced equipment at the State Key Laboratory of Biotherapy in Sichuan and Qin's team, experienced in animal tests, conducted them.
Fifteen hours of work every day, years of accumulated materials research, and clinical experience in bone surgery started to pay off.
Researchers working on 3-D printing at Hong Kong universities recommended Hu turn to precision 3-D printing to build her scaffold. The bone injuries were scanned to determine the shape of the injury, and the 3-D printer built a scaffold that fit precisely.
The big question is can the "broken mirror" be repaired without cracks. The bone scaffold can repair bones without cracks. That's not a complete answer. There remains the question of what happens when the device disintegrates slowly within the body. Will there be side effects? That will take three to five years to discover.
Xie finished her doctoral thesis defence at the end of last year. She's now teaching at College of Textiles and Garments of Southwest University in Chongqing, where she can pass down what she learned across the boundary back to where she started her career.
Contact the writer at dara@chinadailyhk.com

(HK Edition 11/23/2018 page8)